- Lipids in cardiovascular disease play a crucial role in the overall health of our cardiovascular system. Understanding the definition and importance of lipids is essential in comprehending their impact on heart health and the body as a whole.
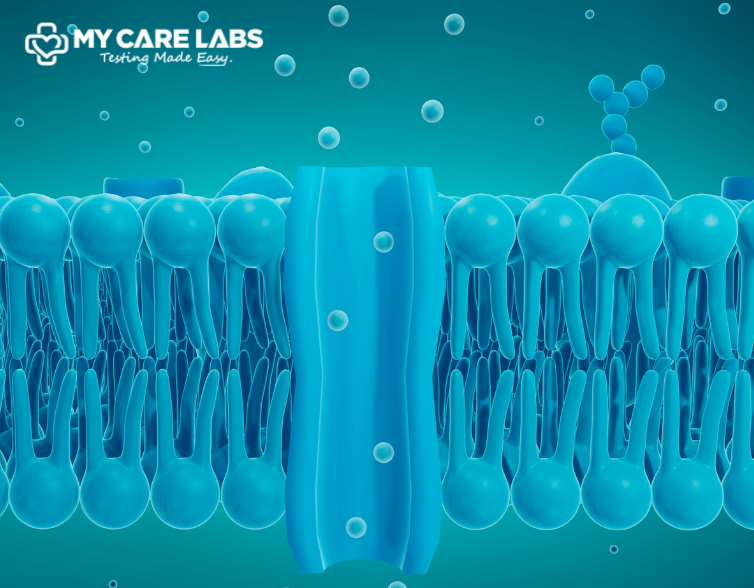
- Lipids, including cholesterol and triglycerides, are fundamental components of cell membranes and play a vital role in various physiological processes.
- They serve as energy sources, aid in hormone production, and support the absorption of fat-soluble vitamins.
- However, an imbalance or abnormal levels of lipids can contribute to lipids in cardiovascular diseases such as atherosclerosis, coronary artery disease, and stroke.
- Lipid profile testing is a key diagnostic tool used to assess an individual’s risk of developing lipids in cardiovascular disease.
- This test measures various lipid parameters, including total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides.
- Evaluating these lipid levels helps healthcare providers identify potential risks and formulate appropriate management strategies.
- An elevated level of LDL cholesterol, often referred to as “bad” cholesterol, is associated with an increased risk of atherosclerosis and coronary artery disease. Conversely, higher levels of HDL cholesterol, known as “good” cholesterol, are protective against cardiovascular events.
- Regular lipid profile testing is recommended for individuals with risk factors such as obesity, diabetes, hypertension, and a family history of lipids in cardiovascular disease.
- By monitoring lipid levels and implementing lifestyle modifications such as a heart-healthy diet, regular exercise, smoking cessation, and medication, when necessary, individuals can effectively manage lipids in cardiovascular disease and reduce their risk of heart-related complications.
I. Understanding Lipids
- Lipids play a crucial role in cardiovascular health, influencing various aspects of heart function and disease risk. By delving deeper into the types of lipids, their functions, and their impact on lipids in cardiovascular disease, we can better comprehend the intricate relationship between lipids and heart health.
Types of Lipids
- Cholesterol: Cholesterol is a type of lipid that is essential for building cell membranes and producing hormones like estrogenic and testosterone. However, an excess of cholesterol, especially LDL cholesterol, can lead to the development of atherosclerosis and increase the risk of lipids in cardiovascular disease. Monitoring cholesterol levels through lipid profile testing is key to managing cardiovascular health.
- Triglycerides: Triglycerides are another type of lipid found in the bloodstream. They are the most common type of fat in the body and serve as a source of energy. Elevated triglyceride levels are often associated with metabolic disorders and can contribute to lipids in cardiovascular disease risk when combined with other lipid abnormalities.
- LDL (Low-Density Lipoprotein) and HDL (High-Density Lipoprotein): LDL cholesterol is often referred to as “bad” cholesterol because it can accumulate in the arteries, leading to plaque formation and narrowing of blood vessels. On the other hand, HDL cholesterol, known as “good” cholesterol, helps remove excess cholesterol from the bloodstream, reducing the risk of plaque buildup and lipids in cardiovascular disease.
Functions of Lipids in the Body
- Lipids play diverse roles in the body beyond energy storage and hormone production.
- They contribute to cell structure and integrity, aid in nutrient absorption (such as fat-soluble vitamins), and function as signalling molecules that regulate various physiological processes.
- However, imbalances in lipid levels can disrupt these functions and contribute to lipids in cardiovascular disease development.
Lipid Metabolism and Regulation
- The body tightly regulates lipid metabolism to maintain a balance between synthesis, storage, and utilization. Lipids are transported in the bloodstream via lipoproteins, such as LDL and HDL particles.
- Dietary factors, physical activity, genetics, and hormonal influences can all impact lipid metabolism and contribute to lipid abnormalities associated with lipids in cardiovascular disease.
II. Lipids and Cardiovascular Disease
Atherosclerosis: The Role of Lipids in Plaque Formation
- Atherosclerosis is a progressive condition characterized by the buildup of plaque in the arteries, leading to narrowing and hardening of the blood vessels.
- Lipids, particularly LDL cholesterol, play a significant role in the development of atherosclerosis. Excess LDL cholesterol can infiltrate the arterial walls, triggering an inflammatory response and the formation of fatty deposits, known as plaque.
- As plaque accumulates, it can restrict blood flow to vital organs, including the heart, brain, and extremities. This narrowing of arteries (stenosis) increases the risk of cardiovascular events such as heart attacks, strokes, and peripheral artery disease.
Lipid Accumulation and Arterial Blockages
- The accumulation of lipids, especially cholesterol, within arterial walls contributes to the formation of arterial blockages.
- These blockages can impede blood flow and oxygen delivery to tissues and organs, leading to ischemia (lack of blood supply) and tissue damage.
- In coronary arteries, blockages can result in angina (chest pain) or myocardial infarction (heart attack) if a plaque ruptures and causes a blood clot to form.
Link Between Lipids, Hypertension, and heart disease.
- Lipid abnormalities, such as high LDL cholesterol and triglyceride levels, are often associated with other cardiovascular risk factors, including hypertension (high blood pressure) and diabetes.
- The combination of these risk factors significantly increases the likelihood of developing heart disease, stroke, and other vascular complications.
- Moreover, lipid-lowering therapies, such as statins, have demonstrated efficacy in reducing cardiovascular events and mortality by lowering LDL cholesterol levels and stabilizing plaque in at-risk individuals.
- However, individualized treatment plans based on comprehensive lipid profiles and overall cardiovascular risk assessments are crucial for optimizing outcomes and preventing disease progression.
III. Lipid Profile Testing
- Lipid Profile Testing is a crucial component of assessing cardiovascular health as it provides valuable insights into an individual’s lipid levels and their impact on overall well-being.
- In this section, we will delve into the importance of lipid profile tests, the components of a lipid panel, interpretation of lipid profile results, and the various risk factors associated with dyslipidaemia and lipids in cardiovascular disease.
Importance of Lipid Profile Tests
- Lipids, including cholesterol and triglycerides, play a significant role in the lipids in health and disease.
- Monitoring lipid levels through lipid profile tests is essential for evaluating lipids in cardiovascular disease.
- Elevated levels of certain lipids, such as LDL cholesterol and triglycerides, can contribute to the development of lipids heart disease and other cardiovascular conditions.
- On the other hand, maintaining optimal levels of HDL cholesterol is associated with a lower risk of lipids heart disease. Therefore, lipid profile testing is instrumental in assessing lipid status and guiding preventive measures and treatment interventions to promote heart health.
Components of a Lipid Panel
Total Cholesterol:
Total cholesterol is a measure of the overall amount of cholesterol in the bloodstream. It includes LDL cholesterol, HDL cholesterol, and a portion of triglycerides.
Elevated total cholesterol levels, especially when driven by high LDL cholesterol and triglycerides, can indicate an increased risk of lipids heart disease.
LDL Cholesterol:
LDL cholesterol, often referred to as “bad” cholesterol, is a major contributor to the buildup of plaque in the arteries, leading to atherosclerosis and increased lipids in cardiovascular disease.
Lowering LDL cholesterol levels is a key target in preventing heart disease.
HDL Cholesterol:
HDL cholesterol, known as “good” cholesterol, plays a protective role by transporting cholesterol away from the arteries to the liver for processing and removal from the body.
Higher levels of HDL cholesterol are associated with a reduced risk of lipids heart disease.
Triglycerides:
Triglycerides are a type of fat found in the blood. Elevated triglyceride levels, often seen in conjunction with high LDL cholesterol and low HDL cholesterol, can contribute to atherosclerosis and heart disease risk.
Interpretation of Lipid Profile Results
Optimal Levels:
Optimal lipid levels typically include:
– Total cholesterol: Less than 200 mg/dL
– LDL cholesterol: Less than 100 mg/dL (lower for individuals at elevated risk)
– HDL cholesterol: Greater than 60 mg/dL
– Triglycerides: Less than 150 mg/dL
Achieving and maintaining these optimal levels is essential for promoting heart health and reducing the risk of lipids in cardiovascular disease.
Risk Factors Associated with High or Low Lipid Levels:
- Elevated levels of LDL cholesterol and triglycerides, along with low levels of HDL cholesterol, are considered major risk factors for heart disease and stroke.
- These lipid abnormalities can be influenced by numerous factors, including genetics, diet and nutrition, physical activity levels, smoking, alcohol consumption, and underlying medical conditions such as diabetes, hypertension, and obesity.
IV. Risk Factors for Dyslipidaemia and Cardiovascular Disease
- Genetics and Family History
Genetics play a significant role in determining an individual’s lipid profile and susceptibility to dyslipidaemia and lipids in cardiovascular disease.
Family history of high cholesterol or heart disease can increase the likelihood of lipid abnormalities and cardiovascular events.
Understanding genetic predispositions can help healthcare providers tailor screening and management strategies for at-risk individuals.
- Lifestyle Factors
- Diet and Nutrition:
The impact of diet and nutrition on lipid levels is well-established.
Diets high in saturated fats, trans fats, and cholesterol can raise LDL cholesterol levels, while diets rich in fruits, vegetables, whole grains, and healthy fats (e.g., monounsaturated, and polyunsaturated fats) can help lower LDL cholesterol and triglycerides and increase HDL cholesterol.
- Physical Activity:
Regular physical activity plays a crucial role in lipid metabolism and cardiovascular health.
Exercise helps lower LDL cholesterol and triglycerides, increase HDL cholesterol, improve overall lipid profile, and reduce the risk of lipids heart disease.
- Smoking and Alcohol Consumption:
Smoking tobacco and excessive alcohol consumption can adversely affect lipid levels and contribute to lipids in cardiovascular disease.
Quitting smoking and moderating alcohol intake can lead to improvements in lipid profiles and heart health.
- Medical Conditions
- Diabetes:
Diabetes, particularly type 2 diabetes, is often associated with dyslipidaemia characterized by elevated triglycerides, low HDL cholesterol, and abnormal LDL cholesterol particles.
Proper management of diabetes, including blood sugar control and lifestyle modifications, is crucial for optimizing lipid levels and reducing lipids in cardiovascular disease.
- Hypertension:
High blood pressure is a significant risk factor for heart disease and stroke. It can also impact lipid metabolism, leading to adverse changes in lipid levels.
Controlling blood pressure through medication, lifestyle changes, and regular monitoring is essential for overall cardiovascular health.
- Obesity:
Obesity is intricately linked to dyslipidaemia, characterized by elevated LDL cholesterol, triglycerides, and decreased HDL cholesterol.
Weight management strategies, including diet modifications, physical activity, and medical interventions, when necessary, can help improve lipid profiles and reduce lipids in cardiovascular disease.
V. Impact of Lipid Management on Cardiovascular Health
- Lipid management plays a crucial role in maintaining cardiovascular health and preventing the progression of lipids in cardiovascular disease.
- Here’s an in-depth discussion on the impact of lipid management and lipid-lowering strategies:
Role of Diet and Lifestyle Modifications
- Proper dietary choices and lifestyle modifications can significantly impact lipid levels and cardiovascular health.
- The consumption of a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats such as omega-3 fatty acids can help lower LDL cholesterol levels and reduce the risk of atherosclerosis and heart disease.
- Incorporating dietary fibre, plant sterols, and antioxidants can also contribute to improved lipid profiles and overall cardiovascular well-being.
- Regular physical activity is another essential component of lipid management. Exercise helps increase HDL cholesterol (the “good” cholesterol) levels, improve blood circulation, and promote heart health.
- Aerobic exercises like walking, jogging, swimming, and cycling are beneficial for cardiovascular fitness and lipid control.
- Additionally, maintaining a healthy weight through a combination of healthy eating and regular exercise can further support lipid management and reduce lipids in cardiovascular disease.
Medications for Lipid Control
- When lifestyle modifications alone are insufficient to achieve optimal lipid levels, medications may be prescribed to help control lipids and reduce cardiovascular risk.
- Several classes of medications are commonly used for lipid management:
- Statins: Statins are widely prescribed to lower LDL cholesterol levels by inhibiting the enzyme involved in the lipids in cholesterol production in the liver.
- They are highly effective in reducing the risk of heart attacks, strokes, and cardiovascular events in individuals with elevated LDL cholesterol levels.
- Fibrates: Fibrates work by lowering triglyceride levels and increasing HDL cholesterol levels. They are often used in combination with statins or as an alternative for individuals with high triglycerides and low HDL cholesterol.
- PCSK9 Inhibitors: PCSK9 inhibitors are a newer class of medications that help lower LDL cholesterol levels by targeting a specific protein involved in the lipids in cholesterol metabolism.
- They are typically used in individuals with familial hypercholesterolemia or those at elevated risk of cardiovascular events despite optimal statin therapy.
Importance of Regular Monitoring and Follow-up
- Regular monitoring of lipid levels through blood tests is essential to assess the effectiveness of lipid-lowering interventions and adjust treatment plans as needed.
- Lipid profiles, including total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides, should be checked regularly according to established guidelines based on individual lipids in cardiovascular disease factors.
- Follow-up visits with healthcare providers allow for ongoing evaluation of lipid management strategies, medication adherence, lifestyle modifications, and overall cardiovascular health.
- These follow-ups help ensure that lipid levels are maintained within target ranges and that any changes or adjustments in treatment are made promptly to optimize cardiovascular outcomes.
VI. Lipid-Lowering Strategies
- Dietary Approaches
- The impact of diet on lipid levels and cardiovascular health cannot be overstated. Dietary approaches aimed at lowering LDL cholesterol and triglycerides while increasing HDL cholesterol include:
- Mediterranean Diet: The Mediterranean diet emphasizes whole foods such as fruits, vegetables, nuts, legumes, whole grains, fish, and olive oil.
- It is rich in monounsaturated fats, omega-3 fatty acids, and antioxidants, making it beneficial for reducing LDL cholesterol and improving overall heart health.
- Low-Fat and Low-Cholesterol Diets: Limiting saturated fats, trans fats, cholesterol, and processed foods can help lower LDL cholesterol levels.
- Choosing lean proteins, opting for plant-based fats, and reducing intake of high-fat dairy products and fried foods are key principles of low-fat and low-cholesterol diets.
- Exercise and Physical Activity Guidelines
- Regular physical activity is a cornerstone of cardiovascular health and lipid management.
- Exercise helps lower LDL cholesterol, increase HDL cholesterol, improve blood flow, and enhance overall cardiovascular fitness.
- The American Heart Association recommends at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise per week, along with muscle-strengthening activities on two or more days per week, for optimal heart health.
- Smoking Cessation Programs
- Smoking is a major risk factor for lipids in cardiovascular disease and can negatively impact lipid levels.
- Quitting smoking or participating in smoking cessation programs can lead to significant improvements in lipid profiles, blood pressure, and overall cardiovascular health.
- Counselling, support groups, nicotine replacement therapies, and medications can be effective strategies in helping individuals quit smoking and reduce their lipids in cardiovascular disease.
VII. Lipids and Specific Cardiovascular Conditions
- Lipids play a crucial role in the lipids in cholesterol metabolism, and their levels can significantly impact both health and disease outcomes, particularly in cardiovascular conditions.
- Understanding the intricate relationship between lipids and specific cardiovascular conditions, as well as lipid management across different patient populations, is essential for comprehensive healthcare strategies.
- A. Coronary Artery Disease (CAD)
- Coronary Artery Disease (CAD) is a common cardiovascular condition characterized by the narrowing or blockage of coronary arteries due to the buildup of cholesterol and other lipids.
- Elevated levels of LDL cholesterol, often referred to as “bad” cholesterol, contribute to plaque formation in the arteries, leading to atherosclerosis and increased risk of heart attacks and angina.
The role of lipids in cholesterol metabolism becomes critical in CAD management. Lipid-lowering medications, such as statins, are commonly prescribed to reduce LDL cholesterol levels and prevent further plaque buildup.
Additionally, lifestyle modifications, including a heart-healthy diet low in saturated fats and regular exercise, play a vital role in managing lipids in heart disease.
- B. Stroke and Transient Ischemic Attack (TIA)
- Stroke and Transient Ischemic Attack (TIA) are cerebrovascular conditions that can result from atherosclerosis and lipid-related factors.
- Elevated levels of LDL cholesterol and triglycerides, coupled with low levels of HDL cholesterol (“good” cholesterol), contribute to the formation of blood clots and blockages in cerebral arteries, leading to ischemic strokes or TIAs.
- Lipids in health and disease are intricately linked to stroke risk. Controlling lipid levels through medication adherence, dietary modifications, and regular monitoring can reduce the risk of recurrent strokes or TIAs.
- Antiplatelet medications and blood thinners may also be prescribed to prevent clot formation.
- C. Peripheral Artery Disease (PAD)
- Peripheral Artery Disease (PAD) involves the narrowing or blockage of arteries outside the heart, commonly affecting the legs.
- Lipid accumulation in arterial walls contributes to PAD development, impairing blood flow to the lower extremities and causing symptoms like leg pain, numbness, and poor wound healing.
- Managing lipids in heart disease extends to PAD management, focusing on reducing LDL cholesterol levels and improving overall vascular health.
- Lifestyle changes, such as smoking cessation, exercise programs, and healthy eating habits, are fundamental in PAD treatment. Medications to control lipids and blood pressure may also be prescribed.
VIII. Lipid Management in Different Patient Populations
- A. Adults and Seniors
- Lipid management in adults and seniors is crucial for preventing cardiovascular events like heart attacks and strokes. Regular lipid screenings, along with lifestyle modifications and appropriate medication therapy, are essential components of lipids in cardiovascular disease reduction strategies.
- Monitoring lipids in cholesterol, along with other risk factors such as blood pressure and diabetes, helps tailor treatment plans for optimal outcomes.
- B. Children and Adolescents
- Early lipid management in children and adolescents is vital for establishing healthy lipid levels and reducing the risk of lipids in cardiovascular disease.
- Education on healthy eating habits, physical activity promotion, and regular lipid screenings are key elements in paediatric lipid care.
- Identifying and addressing lipid abnormalities early can prevent long-term complications and promote lifelong heart health.
- C. Pregnant Women and Lipid Health
- Pregnant women may experience changes in lipid metabolism, with elevated triglyceride levels being common.
- Monitoring lipid levels during pregnancy is important to assess lipids in cardiovascular disease and ensure maternal and fatal health. Lifestyle interventions, such as a balanced diet and regular physical activity, can help manage lipids in pregnancy.
- Close collaboration between obstetricians and lipid specialists is essential for optimizing lipid health during this critical period.
IX. Role of Lipid Testing in Clinical Practice
- The role of lipid testing in clinical practice is paramount in the prevention, diagnosis, and management of lipids in cardiovascular disease.
- Lipids play a crucial role in cardiovascular health, and understanding their levels through lipid testing provides valuable insights into an individual’s risk profile.
- Let’s delve into the various aspects of lipid testing and its significance in clinical practice.
- Lipid Screening Guidelines
- Lipid screening guidelines are essential tools in identifying individuals at risk of lipids in cardiovascular disease.
- These guidelines recommend regular lipid profile testing to assess levels of cholesterol, triglycerides, LDL cholesterol, and HDL cholesterol. The results of lipid testing help healthcare providers evaluate a patient’s lipid status and determine appropriate interventions to reduce lipids in cardiovascular disease.
- Integrating Lipid Testing into Routine Health Assessments
- Integrating lipid testing into routine health assessments is an initiative-taking approach to cardiovascular health.
- Healthcare providers often include lipid profiles as part of routine check-ups, especially for patients with risk factors such as obesity, diabetes, hypertension, and family history of lipids in cardiovascular disease.
- By incorporating lipid testing into regular health assessments, clinicians can detect lipid abnormalities early and initiate timely interventions.
- Patient Education and Empowerment
- Patient education and empowerment are crucial components of lipid testing in clinical practice.
- Patients need to understand the significance of lipid levels in cardiovascular health and the implications of abnormal lipid profiles.
- Healthcare providers play a vital role in educating patients about lifestyle modifications, medication adherence, and follow-up lipid testing to optimize cardiovascular outcomes.
X. Emerging Trends in Lipid Research and Treatment
- Novel Therapies for Lipid Control
- Advances in lipid research have led to the development of novel therapies for lipid control.
- These therapies target specific pathways involved in lipid metabolism, offering more personalized treatment options for patients with dyslipidaemia and lipids in cardiovascular disease risk.
- Novel lipid-lowering medications, such as PCSK9 inhibitors and RNA-based therapies, show promise in effectively reducing LDL cholesterol levels and improving cardiovascular outcomes.
- Precision Medicine Approaches
- Precision medicine approaches leverage genetic and biomarker data to tailor lipid management strategies to individual patients.
- Genetic testing helps identify genetic variants associated with lipid metabolism and cardiovascular risk, guiding healthcare providers in selecting the most appropriate lipid-lowering therapies.
- Precision medicine also considers other factors like lifestyle, comorbidities, and medication tolerance, ensuring personalized and effective lipid control.
- Telemedicine and Remote Lipid Management
- Telemedicine and remote lipid management are emerging trends that enhance access to lipid testing and cardiovascular care.
- Telehealth platforms enable patients to undergo lipid testing at home or local laboratories, with results transmitted securely to healthcare providers for interpretation.
- Remote lipid management programs utilize teleconsultations, digital health tools, and electronic health records to monitor lipid levels, medication adherence, and lifestyle modifications, promoting continuous lipids in cardiovascular disease management.
XI. Common Misconceptions about Lipids and Cardiovascular Health
- Dietary Fat Myths
- One common misconception is the belief that all dietary fats are harmful to lipids in cardiovascular disease.
- While saturated and trans fats should be limited, unsaturated fats, especially omega-3 fatty acids found in fish, nuts, and seeds, have cardiovascular benefits and are essential for overall health.
- Overemphasis on Total Cholesterol Levels
- Another misconception is the overemphasis on total cholesterol levels alone in assessing lipids in cardiovascular disease.
- It’s important to consider the entire lipid profile, including LDL cholesterol, HDL cholesterol, and triglycerides, as well as other risk factors like blood pressure, diabetes, smoking, and family history, to accurately evaluate cardiovascular risk.
- Importance of Considering Overall Cardiovascular Risk
- A critical misconception is focusing solely on lipid levels without considering overall lipids in cardiovascular disease.
- Cardiovascular risk assessment tools, such as the Framingham Risk Score or ASCVD Risk Estimator, integrate lipid levels with other risk factors to estimate an individual’s 10-year risk of developing cardiovascular events.
- This comprehensive approach helps healthcare providers make informed decisions about lipid management and preventive strategies.
- Long-Term Monitoring and Maintenance
- Lipid management is not a one-time intervention but rather a lifelong commitment to maintaining optimal lipids heart disease.
- Long-term monitoring and maintenance play a crucial role in sustaining the benefits of lipid-lowering interventions and preventing disease progression.
- Regular follow-up appointments, lipid profile tests, and lifestyle assessments are essential components of long-term lipid management.
- Patients like Sarah, who successfully lowered her triglyceride levels through dietary modifications and medication adherence, understand the importance of continuous monitoring.
- Sarah’s healthcare team at My Care Labs regularly reviews her lipid profile, adjusts her treatment plan as needed, and provides ongoing guidance on healthy living habits.
- This initiative-taking approach to long-term lipid management has allowed Sarah to sustain her improved lipid levels and reduce her risk of cardiovascular complications.
XII. Future Directions in Lipid Research and Treatment:
- Genetics and Personalized Lipid Therapy
- The future of lipid management lies in personalized approaches tailored to individuals’ genetic makeup and specific lipid abnormalities.
- Advancements in genetics and genomic testing enable healthcare providers to identify genetic variants associated with lipid metabolism and cardiovascular risk.
- Personalized lipid therapy utilizes this genetic information to prescribe targeted interventions that optimize lipids in cholesterol levels and reduce the risk of lipids heart disease.
- Targeted Therapies for Specific Lipid Abnormalities
- As our understanding of lipids in health and disease continues to evolve, targeted therapies for specific lipid abnormalities are emerging as promising treatment options.
- For instance, novel medications that selectively target triglycerides or address genetic lipid disorders are being developed.
- These targeted therapies offer precise interventions that address underlying lipid imbalances and improve cardiovascular outcomes.
- Public Health Initiatives for Cardiovascular Risk Reduction
- In addition to individualized approaches, public health initiatives play a vital role in addressing lipids heart disease at a population level.
- Public health campaigns promote awareness of cardiovascular risk factors, encourage healthy lifestyle choices, and advocate for policy changes that support heart-healthy environments.
- Collaborative efforts between healthcare organizations, government agencies, and community stakeholders are essential for implementing effective public health strategies that reduce lipids in cardiovascular disease and improve lipid profiles in the population.